As CEO of Access Health, Jeff Fortenbacher’s nonprofit tries to provide better health care by offering lower cost health insurance, and providing counseling and care to low income and minority patients around Muskegon, Mich., where the rate of full vaccination in that population is at a mere 14%.
He says the challenges of reaching these communities has gotten even harder lately.
“It just cuts across that whole issue of trust, and suspicion and not getting the information,” he says. After two years of masking, isolation, travel and vaccine recommendations, many are just checked out. “I mean, it’s almost like white noise.”
Even as the omicron variant wreaks havoc on hospitals and COVID kills over 1,500 Americans every day, public health leaders are struggling to get people to tune in to guidance that could help stem the contagion.
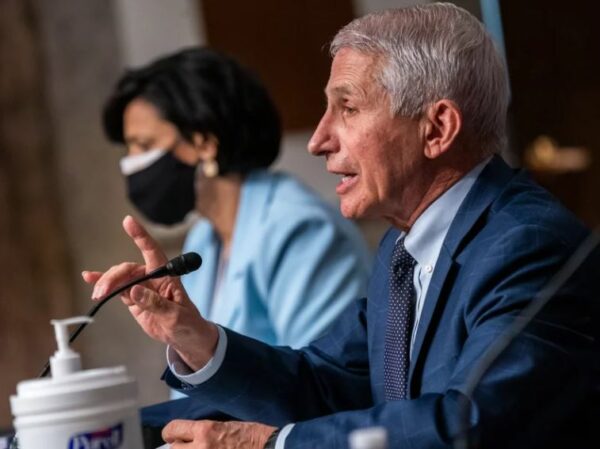
Meanwhile, politicians are pointing fingers at the White House, saying they’re botching pandemic messaging. Senators from both parties grilled Biden administration health officials about their communication strategies Tuesday.
“Most Americans can’t make heads or tails of anything coming out of this administration,” said Republican Senator Tommy Tuberville of Alabama.
Public health advocates acknowledge fewer people are paying attention or heeding expert advice. Many — including White House officials — concede they’re now adapting their messages to the realities of a population with a waning appetite for warnings and mandates. Some say the messaging needs to shift to become shorter, simpler, and even nod to a brighter future when the pandemic is over.
The risk of Americans tuning out during a surge, of course, is that it could prolong the pandemic, says Adriane Casalotti, chief of government and public affairs for the National Association of County and City Health Officials.
“They might be done with the pandemic, the pandemic’s not done with them,” she says.
Among patients and even for himself, Fortenbacher says the fatigue is palpable. “It’s just becoming very draining — emotionally draining, and it’s very politicized — and people are just getting tired,” he says.
The problem with COVID messaging, of course, is that the pandemic is not simple to understand. And public health recommendations are based on an evolving understanding of new science, so messages are necessarily complex and they change frequently.
Normally, whether it’s seat-belt recommendations or smoking cessation, messages do not change often. Yet even consistent messages take time for the public to absorb.
“The challenge we always have with communications, they always say people need to hear things seven times before it really sticks,” says Georges Benjamin, executive director of the American Public Health Association.
The role of vaccination has been particularly difficult to communicate, says Fortenbacher. Those who are fully vaccinated are far less likely to die or get hospitalized. But during omicron, COVID case loads are climbing and the fact that vaccinated people are getting infected at all seems to contradict a common, though inaccurate, notion that COVID vaccines block infections.
“I think that’s confusing for people, is that that initial message was that to get the vaccine, you’re going to be OK,” Fortenbacher says. When they hear about breakthrough infections, they falsely assume that undermines the point of the vaccines and ask: “Why should I do it?”
But vaccines also offer an opportunity for more effective messaging, Benjamin says. Vaccines have altered the threat COVID poses to people who are vaccinated, he says, and public health can acknowledge that progress and give people a roadmap for the future, based on how previous pandemics have ended. He argues people might be more receptive to listening to messages, if it’s focused on looking forward.
“There is a reluctance to give people information because we’re afraid of being wrong three months from now, but I think we do need to give people a sense of hope, and we need to tell people what we anticipate going forward and how this ends,” he says.
There are other ways messaging needs to adapt, Fortenbacher says. For instance, in his experience, policies have had to shift to accommodate what is realistic. That means recommending — but not mandating — masks, even in clinics, for example, because requiring them would likely just undercut their health goals by alienating some patients.
“If you require them to mask up, you aren’t going to accomplish what you’re trying to accomplish, because you aren’t going to engage them because they’re going to be so pissed off,” he says. “It’s really kind of just walking that line.”
The country is fielding the consequences of decades of divestment in public health infrastructure, including expertise in messaging, says Deborah Burger, president of the National Nurses United.
“If we had had the foresight to truly fund the public health system … this would have rolled out a lot smoother, because people would be used to listening for the alerts, the updates, and actually know that they could trust it and believe it,” she says.
Casalotti agrees communications is an underfunded function at most state and local public health agencies, which are now struggling with public outreach; in fact, she says, many people have stopped taking their calls.
“They’re not picking up their phone when the contact tracers call them; they are not giving information about who they’ve been in contact with or where they’ve been,” she says, and that hampers health agency’s abilities to follow up and stop the spread.
But, she says, there’s a messaging opportunity here too. People are still interested in what’s happening in their local area, and public health officials should try to capitalize on that.
“If you can talk about your county, if you can talk about your corner of a state and talk about the data in that way to be more specific about what’s actually happening to your friends and neighbors, that’s another way to bring some of these big conversations more to life,” Casalotti says.
Like many others, Casalotti also argues guidance needs to be simpler and easier for the public to comprehend.
“The bumper sticker version is much easier than the three-page version, or even the three-paragraph version,” she says.
9(MDQ2OTU5NjExMDE2MTkwMTE2MDExMzAxYg000))




