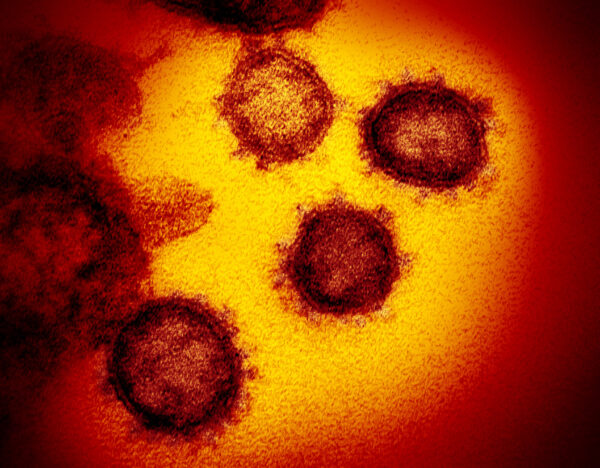
During the early days of the pandemic, scientists and doctors were concerned that being infected with SARS-CoV-2 might not trigger a strong immune response in many people – thus an infection might not provide long-term protection.
“Immunity to Covid-19 could be lost in months, UK study suggests,” a headline from The Guardian alerted back in July 2020. “King’s College London team found steep drops in patients’ antibody levels three months after infection,” the story warned.
But that idea was based on preliminary data from the laboratory — and on a faulty understanding of how the immune system works. Now about a year and a half later, better data is painting a more optimistic picture about immunity after a bout of COVID-19. In fact, a symptomatic infection triggers a remarkable immune response in the general population, likely offering protection against severe disease and death for a few years.
And if you’re vaccinated on top of it, your protection is likely even better, studies are consistently showing.
Here are several key questions people have been asking throughout the pandemic – and ones that researchers are beginning to answer.
If I just had COVID, am I protected against getting a severe course of COVID in the future ?
With SARS-CoV-2, your immune system generates two types of protection: protection against reinfection and protection against severe illness upon that second infection. Let’s start with the latter.
If you’re under age 50 and healthy, then a bout of COVID-19 offers good protection against severe disease if you were to be infected again in a future surge, says epidemiologist Laith Abu-Raddad, at Weill-Cornell Medical-Qatar. “That’s really important because eventually, every one of us will get infected,” he says. “But if reinfections prove to be more mild, in general, it will allow us to live with this pandemic in a much easier way.”
Abu-Raddad and his team have been tracking reinfections in Qatar for more than a year. In one study, the team analyzed about 1,300 reinfections among more than 350,000 people in Qatar. They found that a prior COVID-19 infection reduced the risk of hospitalization upon reinfection by about 90% compared with in people having their first infection.
These findings, published in the New England Journal of Medicine in December, are consistent with data released by the Centers for Disease Control and Prevention last month. In that study, a prior infection reduced the risk of hospitalization during the delta surge by more than 50 times compared with in people who hadn’t had a prior infection and were not vaccinated. People who had had both a prior infection and were vaccinated had the most protection.
And here’s the “really good news,” Abu-Raddad says: This protection against severe disease persists, perhaps for years. “We’ve been following this same group of people for over a year and a half now, we don’t see much waning. If it’s there, it’s too small to discern.”
But the good news doesn’t necessarily hold true for everyone. This long-term protection is seen in healthy people under age 50, Abu-Raddad points out. It’s likely less potent and possibly more short-lived for people who are older or who have underlying health conditions, he says. More data is needed to know how the protection varies with age.
That said, studies in the laboratory also suggest that protection against severe disease is long term after a bout of COVID-19, at least for healthy people.
In particular, antibodies against SARS-CoV-2 persist in the blood for months, possibly years after an infection, scientists at the Fred Hutchinson Cancer Research Center and Emory University have reported.
In that study, immunologist Juliana McElrath and her colleagues measured antibodies in the blood of more than 200 people after a confirmed SARS-CoV-2 infection. More than 90% of the volunteers generated antibodies to SARS-CoV-2 right after the infection. In general, the level of antibodies declined quickly two to three months after an infection, but after about four months, the level began to plateau. Even after eight months, the vast majority of people in the study still had antibodies in their blood that could neutralize SARS-CoV-2.
After publishing that study in Cell Reports Medicine, the team continued to follow these same people, and the team now has data up to 15 months after the infection, the researchers told Nature on Tuesday. So far, the antibodies seem to be sticking around for the long haul, said immunologist Rafi Ahmed at Emory University, who helped to lead the study. “Looking at the shape of the curve, it looks pretty damn good. It is really quite stable.”
Last Tuesday, researchers at the Johns Hopkins Medical Institutions also reported that SARS-CoV-2 antibodies can persist up to 20 months. In that study, 293 out of 295 unvaccinated people generated antibodies after a positive COVID test.
This pattern, with antibodies declining quickly and then plateauing, occurs with any infection, not just SARS-CoV-2, immunologist Deepta Bhattacharya told NPR back in August. “In every single immune response, there is a sharp rise in antibodies, a period of sharp decline,” and then it starts to stabilize at a lower level.
About six months after a SARS-CoV-2 infection, right around the time when the antibody level starts to stabilize, the immune system does something extraordinary: It generates special cells, called long-lived plasma cells, that can make potent antibodies against SAR-CoV-2, for decades, possibly even a lifetime. “These cells are remarkable,” Bhattacharya said. “They’re estimated to spit out something like 10,000 antibody molecules per second.” Therefore, you wouldn’t need many of these cells to protect against a future infection.
On top of that, the immune system also generates several types of cells, known as B and T cells, which kick into action upon reinfection. These cells quickly ramp up antibody levels and destroy infected cells to ensure a mild course of COVID doesn’t turn into a serious one. Several studies, including one published in January, have shown that these cells are durable and likely persist longer than year.
Does this mean I won’t get reinfected if I’ve had COVID or even better, have had COVID and am fully vaccinated?
Unfortunately, the answer is no.
“Reinfections are not just possible, they’re pretty much inevitable,” says evolutionary biologist Jeffrey Townsend at Yale University. “At least all the evidence that we have now says that that’s true.”
To estimate how often reinfections will occur with SARS-CoV-2, Townsend and his team have been studying four other coronaviruses. They are known as “seasonal coronaviruses” and cause about 30% of colds each year.
“They all infect and reinfect on a yearly timescale,” he says, “so there’s no reason to expect something different from SARS-CoV-2.”
The risk of reinfection is likely very low right after you’re sick — up to about four months or so afterwards, Townsend and his team estimate. Then the risk grows. And their data suggest that, on average, people will be reinfected every year or two with SARS-CoV-2. “It is very rare for reinfection to happen on a very short timescale, but on a longer timescale, it seems to happen with some frequency,” he says.
But your specific risk for reinfection depends heavily on your personal situation, such as whether you’re exposed to lots of people at work or live with children who go to school. “So that time frame for reinfection each year or so assumes that we all just relax everything about our protections and just sort of let it rip, basically,” Townsend says.
And, he says, your risk of reinfection also depends on the virus and how much it mutates. For example, during the delta surge, a previous infection offered about 85% protection against reinfection, Laith Abu-Raddad and his team found. But with omicron that protection dropped to 55%. So the chance of reinfection was much higher.
So why is the immune system so good at preventing severe disease but not really able to stop reinfection?
No one knows for sure. But this strategy may be a deliberate one by the immune system, immunologist Jonathan Yewdell explained last week on the podcast This Week In Virology.
In essence, your immune system is allocating resources. And its primary goal is to keep you alive. So the immune system has decided that, with coronaviruses, it’s not worth stopping the infection as long as it can stop serious, life-threatening illness.
“That is good enough under most circumstances,” Yewdell, who’s at the National Institutes of Health, explained. “You might not think when you’re in bed with 106 [degree] fever, you know, and crying for your spouse to help you because you could barely move that ‘this is good enough.’ But as long as you’ve recovered … you know, mission accomplished.”
In other words, the immune system is not built to stop every sickness or asymptomatic infection. And it’s definitely not built to “give you a negative PCR test,” Yewdell says.
So the future of COVID-19 is starting to become clearer: We’re going to have a lot more infections but hopefully a lot fewer hospitalizations and deaths.
Editor’s note: Yewdell’s point about the possible severity of illness figures into the answer to the question: Should you deliberately try to get COVID-19? To read more, see this story.
9(MDQ2OTU5NjExMDE2MTkwMTE2MDExMzAxYg000))




